This week we are continuing our theme of bringing you 25 (more!) ways to improve the patient experience. From enhancing your patient parking to accurately communicating office wait times, this episode is chock-full of advice for keeping your patients happy.
This week we are continuing our theme of bringing you 25 (more!) ways to improve the patient experience. From enhancing your patient parking to accurately communicating office wait times, this episode is chock-full of advice for keeping your patients happy.
There are many different touch-points your patients go through before even seeing a physician, and these are often the factors that can make or break a new doctor-patient relationship. It may seem trivial, but features that have nothing to do with medical care, such as easy parking and updated tech components, can be the deciding factor when deciding to try out a new practice (and are most often the topics people post about on review sites). Updating and personalizing your practice to what your patients want and need will greatly improve your practice’s reputation and result in repeat business.
The patient experience often hinges on small personal touches, like hand-written notes, or customizing your on-hold messaging system. Don’t let your patients feel like they are replaceable. Listen to their concerns – often they just want to feel like they’re in good hands, which starts as early as making that first appointment.
In this week’s episode, Jennifer and Corey discuss ideas to personalize the patient experience, such as providing additional information about the appointment upon arrival. We also suggest ways to make your office more tech-savvy, such as sending text-message appointment reminders, or posting an interactive parking garage video to your website.
If you haven’t already, be sure to check out Part I and Part II for fifty more action-items. And stay tuned for Part IV in the near future!
Tune in to discover:
- How to streamline and modernize your check-in process
- Tips to make parking patient-friendly
- Different ways of scheduling appointments based on customer needs
- How to make your on-hold messaging system more engaging
- Suggestions for dealing with long office wait times
Free Healthcare Awareness 2024 Calendar
Nearly every month of the year has a health holiday or observance, and there are also a number of awareness months that your patients and staff would love to know about. You also don’t want to miss chances to celebrate with your practice’s followers.
Free Healthcare Awareness 2023 Calendar
Nearly every month of the year has a health holiday or observance, and there are also a number of awareness months that your patients and staff would love to know about. You also don’t want to miss chances to celebrate with your practice’s followers.
Transcription Notes
Speaker 1: Dr. Marketing Tips, paging Dr. Marketing Tips. Dr. Marketing Tips, you’re needed in the marketing department.
Speaker 2: Welcome to the Dr. Marketing Tips Podcast, your prescription to the answers you seek to grow your medical practice easier, better and faster. This show is all about connecting practice administrators and medical marketing professionals with peers working in practices, learning from experiences, making mistakes and sharing successes. Let’s get started.
Jennifer: Hey there, welcome to the Dr. Marketing Tips podcast. I am Jennifer.
Corey: And I’m Corey.
Jennifer: And we are here today to continue our series on ways that you can improve the patient experience over at your practice. And we are eyeball deep in patient experience, improvements here at Insight Marketing Group and Insight Training Solutions. Corey, how has your week been?
Corey: In a word, hectic. So just real quick, we are, like Jen said, working on a lot of patient experience initiatives and for one of our clients, we’re actually having a mural painted in one of their practices, one of the main locations. So we’ve gone through this whole big planning process, everything’s getting ready to roll out, we’re supposed to start on a Friday. Wednesday afternoon the mural artist called me and said that he just … he quit basically in the 11th hour because too many changes and whatnot. So that sent us into a panic and a frenzy that pretty much ruined the rest of the week. So recovering from that. But other than that, I’m peachy.
Jennifer: Yeah, working with artists can be … it can be great, and it can be difficult at times too. The creative types. Yeah. I was in Austin, Texas this past week. Went in on Sunday afternoon, attended the MGMA Operations Conference on Monday and then on Tuesday morning gave my social media customer service talk to about 150 practice managers. And I will tell you that between my conversations with the practice managers and a handful of physicians at the conference, as well as the sessions I attended, patient experience and improving patient experience at the practice level is top of mind right now across the entire industry. So I’m excited to share-
Corey: It’s a big deal.
Jennifer: Yeah, absolutely. And I’m excited to share some of these kind of tips as we continue the series, because I think the series is going to end up being a real resource for some of the practices that we work with. So let’s go ahead and dive right into it. so I think we left off talking about billing and records and let’s go ahead and get started with what do you think we can do to improve the experience maybe in the check-in process?
Corey: Yeah, I think one of the things that we’ve seen and we’ve heard from folks that we work with is a big area for improvement for a lot of practice is kind of improving that process for every generation of patient when they go to check in. Specifically we’re talking about as someone comes through the doors, they’re going to expect different things. For example, I would be fine because I’m a little bit younger, with an iPad to check in. I honestly, I probably would be fine if I didn’t have to talk to someone and I could just do it myself and it told me what to do and where to sit, not a big deal. But obviously if you’re going to talk to someone who’s 75, they are not going to be okay with that experience. So I would say one option is just make sure depending on who the patient is, just be sure to have different ways that they can actually check in that they are comfortable with.
Jennifer: Yeah, I totally agree. I even think, and this was talked about quite a bit at the MGMA because there were a bunch of new tools that folks are starting to use to make the process a little bit easier and there was a discussion that it would be great if we could actually use the portal for what it’s been intended for and allowing individuals who want to check in, pre-check in via the portal, to have all of their information filled out and ready to go so that you’re not having to repeat the process when you get to the practice. And that’s kind of my next piece on how could you improve the patient experience, is to look at your protocols and the processes you have in place for checking patients in.
Jennifer: And let’s not keep asking patients for the same information over and over again. Because I think especially when you’re working with a younger generation, we’re just not … and I’m going to say “We” because I feel like I have one foot in the younger generation and one foot in the much older generation, but we’re all kind of tired of having to jump through hoops when they’re unnecessary. And when you’re repeating yourself on paperwork all the time, or not seeing what you’re doing online transferring over to the actual in office experience, it’s frustrating and it’s ready to make us just kind of stop and find a doctor who’s a little more up with the times.
Corey: Well, yeah, if you look at anything with the way that the world is going now, Uber, and Door Dash and these food delivery systems, we sort of are evolving into a society that expects and wants everything right away. And so to then have to spend all this time on the paperwork, go into the office and have someone not communicate well enough, whether it’s the software or it’s actual people in the office, whatever the case may be, then to have to do all the stuff again, it’s like everything else is moving towards this sort of fast-paced environment and then this, it just feels like it’s stuck in 1995.
Jennifer: Yeah, I was listening to a practice manager that was doing a case study on some text-based application that they had implemented at their practice. It was an OBGYN practice in north Florida. And it was interesting because the practice manager said after they implemented this new text-based service that he now goes to the practice website if he’s looking for a new provider for himself or his family, and he specifically looks at the website and takes that as kind of a first impression to whether or not that practice is going to be up on the times. And so that his experience and outcomes there, non-medical related outcomes, but his overall experience, he feels like if the practice’s website is modern and the doctor seems like they’re hip and they’re on top of it, maybe they have a chat functionality and he can schedule his appointment online, that that might translate to his experience in the practice as well. He doesn’t want to go to antiquated practices anymore. And it was interesting to hear that after they implemented this text-based messaging for patients at his practice that it’s changed the dynamic for him when he’s looking for providers of his own.
Corey: It changed his perspective.
Jennifer: Absolutely.
Corey: Yeah, and it makes sense. We say that all the time. The website’s kind of like a living brochure. So you want to put your best foot forward. And if you’re not, then you wind up in a situation like that. Alright, so my next tip for the check-in process as it relates to patient experience is just be informative. And for that, if someone is asking a question when they come in, either … If the front desk people … We don’t expect them to be trained and know the answer to everything, but at least know where to go to get that answer. And in that same regard, I can’t tell you the amount of times that I’ve been to a physician’s office and you’re handed that new patient paperwork and they tell you what to fill out, what not to fill out, but there’s nothing … I don’t think I’ve ever seen anything in those packets that says “What’s going to happen to me?” It would be nice if as I’m sitting there and filling those things out, tell me more about the practice, the physician, the process. Just give me all the information. And whether I use it or not, that’s up to me. But I don’t think I’ve ever even been presented with that option.
Jennifer: You’re hitting the nail on the head for me. And I know I keep referencing these talks that I was participating in at this conference this past week, but there was a discussion about the idea of checking a patient in and not just having them go sit somewhere. Because when they’re sitting there, their mind is wandering. And so there was a practice that was talking about their reputation scores and how they were getting negative feedback from patients because they felt like nobody was paying attention to them and they were waiting longer than maybe they thought they should. So they changed their process at check-in so that the person that … They send them to the waiting room and then a person comes and gets them.
Jennifer: And instead of just opening the door to the patient room and sitting them in there by themselves, the person will walk into the patient room with them and go over some basic information inside the patient room. And then because of that extra touchpoint of walking in there with them, it changed the perception of the patient and the reputation scores went up. And all they did was make an adjustment of where they were getting the information, instead of out in another room, they did it in that personal setting so the person felt that they had their attention and they hadn’t even seen the provider yet. So I think you’re right. You just have to be informative and tell people what to expect.
Corey: Yeah, it feels like a real conversation, which is really all you want. You want to be heard and you want to have this quick connection and get your questions answered and if you can do that in 45 seconds, then fantastic.
Jennifer: Absolutely. And I think overall, even though we’re all busy, that you’re okay with waiting a little bit, but you need to know why you’re waiting and what the expectation is.
Jennifer: If you like what you’re hearing and need some help marketing your medical practice this year, be sure and check us out at insightmg.com. That’s insight, M as in marketing, G as in group, dot com. Don’t think you’ve got a budget for this kind of stuff? Think again. We’ve got you covered. Make sure you schedule a free consult today.
Jennifer: So that goes into the next one. I’m going to say at check-in, once you check somebody in, you need to be available to them. You need to know their name, you need to make eye contact. If somebody has a question, you need to be able to answer that question. You don’t ignore a patient once they’ve checked in. It is your responsibility to make that patient comfortable until they go into the next piece of the process.
Corey: Weren’t you saying that the hotel that you checked into when you went to Austin, they had someone walking around with water, right?
Jennifer: So for our listeners, we live in central Florida. We’re the number one tourist destination in the world, so I have a very high expectation for hospitality. So when I was in Austin I had the opportunity to stay at the Fairmont and I had never heard of the Fairmont before. It’s a brand new hotel in Austin. And I looked them up and they’re known for their concierge service. But before I looked them up, we got there and we’d been flying for several hours. Actually my flight … I had to be at the airport at 5:20 AM. That was takeoff. So we were at the airport by 4:00. So by this time we’re kind of grudgey and tired and we’re in line with a bunch of other people to check in and they have people walking around with cold bottles of water. And what an experience and that set the tone for the entire couple of days that I was there. So what could you take from something as simple as a bottle of water back to your practice to make an impact on your patients?
Corey: Exactly, that’s why I brought that up because I was just thinking what a small thing to do that makes a big difference because when you came back you told all of us about that and how that was your first impression of the hotel. So it’s interesting-
Jennifer: And I talked to a lot of people.
Corey: Yeah, exactly. The small things make a big difference.
Jennifer: I mean, I talked to random strangers about that kind of stuff. Alright, alright. Let’s go to the next one. Parking. What’s going on with parking and how can you improve the patient experience there?
Corey: So I think this is an area where people … You just kind of … A lot of practices will just put up a couple of signs and they’ll have some physician parking and then you don’t really think about it because honestly, why would you? But it’s important to take into consideration the type of parking that you have too. So Jen just mentioned, we’re in central Florida, which means it gets really hot. And I’ve seen some physician practices where they actually will have covered parking almost all the way through, which is awesome, especially if you have an older population that you know is going to be visiting the office. So just kind of take that into consideration. Make sure you have appropriate parking and ample parking for the folks that are coming in and out of your practice every day. I think that’s an easy one that we can all do and we can sort of set it and forget it.
Jennifer: I agree. And you want it to be in a place that’s comfortable. People feel like it’s safe and not too far away from the building and things like that. I think another one which is often overlooked is we have one client that has parking in a parking garage and I feel as if we’re constantly helping them with new signs or talking about people wandering, trying to figure out where the practice is and it’s because the parking garage can be difficult. So you really need good signage that clearly shows where your office is located and where you’re supposed to park.
Corey: I would say that weekly one of us or someone on our team will run into someone that’s in the wrong spot because they can’t find the office.
Jennifer: I just helped someone the other day.
Corey: Yeah, exactly. And it’s just because the signage isn’t 100% clear. So something that you can do in your practice is park somewhere you wouldn’t normally park and then sort of take a walk and put yourself in the patient’s shoes, like literally. And look at what they’re looking at if it’s not super clear how to get to your office, either think about additional signage that you can use there, or consider creating some sort of online quick video tour type thing that says “When you park, this is where you go,” even if it’s like a quick time lapse video on your iPhone where you’re just walking from your car to the front door, post that on your website, on your social media, because I promise that will make a big difference.
Jennifer: Yeah, I think you’re absolutely right. And I think be wary of signs. When I was-
Corey: Too many signs.
Jennifer: Yeah, too many signs means people won’t read them. And just because you think they are easy to read and understand, they’re not necessarily to read and understand for other people.
Corey: Absolutely.
Jennifer: Cool, what’s your next one.
Corey: I would say it’s important, especially again, if you have … For example, orthopedic practice. So a lot of people that are coming to your practice, they’ve got bad knees, bad hips, bad ankles, et cetera. So consider having a valet option. So we work with one practice. They have this mostly because of kind of a parking overflow situation. They just don’t have enough parking, so they’ve instituted free valet for patients during clinic hours. And that’s a gesture that we have heard time and time again, the patients absolutely love. And again, going back to the reputation scores, one of the things that folks were complaining about became very apparent that parking was an issue because almost every negative review that this practice was getting was in regards to the fact that there was nowhere to park, or they had to park so far away and walk for two minutes or whatever the case may be. So if that’s something that you’ve started to hear, or you just want to kind of go to that extra mile, then consider having complimentary valet for your patients.
Jennifer: Yeah, and do you remember that time … We used to push this practice to get the valet and I felt like every time we went to visit, we would notice that the parking was an issue in the parking lot. And so then the final straw, if you remember, Corey … These are like little old ladies, this is an older generation area, and we’re walking through to go meet with the client and there’s these little old ladies in the parking lot trying with their walkers to get to this orthopedic group. And then this other person who’s a little old lady, but not as little and not as old, they almost got in a fist fight and they’re yelling in the parking lot over a parking space and if that wasn’t the kicker to get the valet, I don’t know what was. And now their reviews and the feedback and the overall experience has improved drastically ever since they just did that one thing of getting the valet in the parking lot. So take those things into consideration and what it means to the patient when they’re frustrated just trying to get to your front door.
Corey: It was almost a beat down with a walker.
Jennifer: It really was. It was good entertainment. I wish we had a video of that because it was pretty funny. And that leads me to the one that just drives me absolutely nuts, and that is about being mindful of where the doctors and the staff park at your practice. Because years ago I was taking my husband to the cardiologist after his heart attack and we were running late and it was a new office of a cardiologist that had been assigned to him. And we get to this place and there’s nowhere to park. And by the time we were up at the front door, I turned and noticed an entire row of parking that was available and every one of the signs in front of those parking spots said that it was reserved for the physicians only. And I’m sorry, it’s supposed to be about your patients, not about your physicians. And I agree, physicians need to have parking and of course it’s important for them to be close to the building, maybe in the back, but you can’t … that’s not the kind of best foot that you want to put forward. It should be about your patients and your staff and your doctors should park away from the front door.
Corey: Yeah, no, that’s a great point. And something that I’ve noticed too, and again, I hate to keep harping on ortho practices, but I just happen to see it there, you can tell what type of a car that a surgeon is driving. Even if it’s not reserved-
Jennifer: Porsche, Jaguar, Mercedes.
Corey: Right. So I see constantly as-
Jennifer: Land Rover.
Corey: [inaudible] in particular that we work with, the entire front of the parking lot, and there is no back parking, it’s only in the front, but it’s full of Porsches and Jaguars and Maseratis and Audis and you know it’s the doctors and you know that everyone that’s coming to see you, like I said earlier, they’ve got bad hips and bad knees-
Jennifer: Or they’re on crutches, wheelchair trying to go up a ramp.
Corey: Right. And I would say maybe eight out of 10 people don’t notice. But there’s probably a car guy that’s going to walk up and put two and two together and go “Wait a minute. This isn’t right. I’m on crutches here and I got to park all the way back there because these guys have to park right up front?” And they immediately come in with a chip on their shoulder and they’re a little upset and it’s a simple, stupid little thing, but that totally could be avoided if you were just mindful of where the doctors are.
Jennifer: Yeah, it’s all about the perception and it so impacts the patient experience. Alright, so let’s go into the next set of things, the ideas that you can use to improve the experience. So let’s talk about appointments.
Corey: Okay, definitely. I think one of the easiest ways to improve the patient experience is to make it easy for the patients to schedule their appointment. And I think the best way to do that is just have multiple different avenues where they can request. So obviously they can call on the phone, they can walk into the office. But online I think there’s a lot of room for improvement for a lot of practices. That can be anything from having just a contact form on your website, maybe it’s just a button that says “schedule” and it sends and email. Some practices are starting to introduce a chat functionality where that’s either automated or it’s actually manned by someone in the practice when they’re available and they can … If it’s automated it might plug right into the EHR. If it’s manual, you might have somebody on the other end that just knows what to do and ask the right questions. Obviously everything is HIPAA compliant and secure and encrypted and all that fun stuff. But I think that’s really the way that the online appointment request is going. So if you want to improve the patient experience and sort of get ahead of the game a little bit, then I would say that chat functionality on the website is a great place to get started.
Jennifer: So when I was at the MGMA Conference this week, I went in on a session where it was a case study on this text-based technology that this OBGYN practice up in north Florida had implemented. And one thing that they were talking about is … or one area that they saw improvement by using the online form for online scheduling where you, as a [inaudible] at 3:00 in the morning go in and schedule your appointment. So you’d pick your appointment slot and then the software will automatically send a text message to you if an earlier appointment slot opens up. So you can, through your phone, change your appointment to get an earlier slot that may not have been your first choice, but having that kind of two-way request option, where you never have to talk with anyone on the phone, just truly integrating technology into requesting the appointment and then even approving the appointment. And they saw something like a 30 percent change in no-shows by being able to do this.
Corey: [inaudible 00:21:32]. That’s awesome.
Jennifer: So I think there’s something to be said about technology. Absolutely. I think another area that you really should focus on from the patient experience standpoint, as simple as it sounds, it’s when you’re doing like a phone confirmation or a phone reminder or even on your website on the appointment page, even maybe it’s your … maybe it’s the automated email that somebody receives when they request an appointment, but giving them directions including landmarks and intersections that are near the office so that when you’re sending them that reminder, maybe it has the directions, physical directions, or maybe that video that you were talking about, Corey, if you’ve got parking that’s hard, maybe if they’ve got it at the office that has interesting or challenging parking, the email responder has access to that or something in there. So if you can get in front of anticipating that they may have directional challenges, that you can get in front of that by just merely asking the patient what their needs are.
Corey: Yeah, and just think if that could save you three no-shows a month, I mean, what is it worth to put in that one sentence in the email, you know?
Jennifer: Absolutely. And those no-shows, it’s frustrating for the patient, it’s frustrating for the physician too. Your job as a practice manager is to fill their schedule and if they’re … If your doctors have time on their hands, they’re going to end up in your office and that is not where you want them, alright?
Corey: Exactly.
Jennifer: Kind of the next one is I think that it’s important as practices, especially as technology evolves, that we are all paying attention to things like following up via text message. Not necessarily just phone, but paying attention to the age or the preferences of the patient. And then making your follow-up process work for that patient. Don’t assume that every patient is going to fit into your mold. You should have options based on where that patient is in their lifecycle.
Corey: Yeah, I don’t want you to call me and tell me that I have an appointment coming up, to confirm it. Honestly, for me, that’s a waste of time for your staff, whoever’s picking up the phone to make that phone call. And then on the user side, I’m not going to answer it probably. And then I have to go check my voicemail. And I know it sounds stupid and it’s first world problems, but if you just sent me text and I could just press Y to confirm, I’m good, you know? So like you said, it matters because different generations would like to receive that information differently. I’m totally fine that way. My mother, for example, would prefer the phone call because she wouldn’t … I don’t even know if she would look at the text, honestly.
Jennifer: Yeah, and I would get a phone call, and I would be like “Well, hell. I don’t have my calendar in front of me to know that I’ve got an appointment next Tuesday.” Now I’ve got to stop what I’m doing, pull up my calendar. I’m with you. So I think you just got to understand your patient and how they want to receive information and then give them the information in the way that they want to receive it.
Jennifer: Hey there. Replacing an employee can be expensive, upward of 50% of that employee’s annual salary. Did you know that only 33% of your employees are actually engaged at work? Well, what if you could invest in engaging and training your employees for as little as $8 per month, with training that’s specific to the challenges you face in your medical practice, like customer service, patient experience, communicating across generations, just to name a few? Well, visit us at insightmg.com to find out more about how our employee engagement and training platform can help you strengthen employee retention, develop patient service mindsets, and give you peace of mind when it comes time for annual reviews, all without creating any additional work for you and it’s only $8 a month. So check us out at insight, M as in marketing, G as in group, dot com. We’ll be waiting for you.
Corey: Yeah, for sure. Alright. So my tip for when it comes time to request an appointment, I think this is super helpful, and again, something that you can do very easily, but set clear expectations for what’s going to happen, especially if you have sort of a unique subspecialty for your practice, let people know what to expect. So are there a lot of forms to complete? Is it going to take me … is this first appointment going to take an hour and a half? Do I need to take off a half day at work? Am I cool thinking it’s just going to be 30 minutes? Does it depend on what time of day my appointment is? Does the doctor get behind? Should I anticipate that? Those little things … And again, they can just be a handful of bullet points before the request is actually made, but that sets the expectation for me as a patient and makes it much more likely that I’m going to have a better experience if I know what’s going to happen on the other end. So rather than just “Great, you scheduled an appointment. Here’s a mountian of forms. Good luck. Show up 15 minutes early.” Well, if you sort of tell me what to expect and again, give me that information and set those expectations, we’re both going to be better off for this in the end.
Jennifer: Perfect. Yeah. I totally agree with you and I just think the appointment process is something that so many practices could improve by just paying attention to who the audience is.
Corey: Yeah, absolutely. And if you improve right there, then you’re off to the races already. You’re on the right foot, everyone’s happier and then you’ll eventually see better outcomes and more full clinic schedules as a result.
Jennifer: Absolutely. So the next area that I’ve been thinking about from a patient experience standpoint and also really from a marketing standpoint is something that gets overlooked so often, and that is your on hold messaging, or your phone process in general because a lot of times people are still picking up the phone, calling the doctor’s office, especially if they have a question, and there’s nothing worse than when you get there and you’re on hold for a bunch of time and it’s dead air, just silence or talk radio or something like that. So I think it’s really important to pay attention and to have on hold messaging that is pleasant to the ear. I think it’s really a positive from a marketing standpoint to update your on hold messaging to communicate the things that are going on in your practice or things that you want patients to know and you can actually have fun with it and use it from a marketing standpoint.
Jennifer: So I think it’s first you want to be pleasant, you want to make sure it’s a pleasant experience on the phone. And then I think following up on that, you want to have the right kind of messaging with the right kind of voice, you want to have some light music that goes with it, and then the last piece from a patient experience standpoint is you want to just really be mindful of how long your patients are going to be on hold and be mindful of that phone tree, because there’s nothing worse than somebody being stuck on a hold for something they could have gotten answered on a chat bot.
Corey: Yeah, if the patient is on hold long enough to hear your entire message repeat then you’re in trouble.
Jennifer: Yeah, same thing with your lobby videos.
Corey: Yes, exactly, exactly. And then I would just very quickly add to that that it’s okay to have varying degrees of messaging there. So you can have some sort of things that are canned and that are always there, but if you have some sort of special event coming up … Like we work with a plastic surgeon. He’s going a hydra facial event. His on hold messaging is the perfect place to advertise that because the people that are calling in most likely are the right people to attend that event. So just kind of keep that top of mind that it doesn’t have to be something where you create this new, big script and then you can forget about it for three years. It’s okay if it changes.
Jennifer: Alright, so the listeners right now is the time to pick up your pen because I’m going to give you a piece of information that you can use on your on hold messaging that will make a big difference and that is to take your patient testimonials that you have already got someone to edit, and when they edit down your next patient testimonial video, have them give you a 15 second audio clip and then take those audio clips and put them into your on hold messaging. So it’s your patients giving their 15 second testimonial of how you’ve changed their life and you’re going to put that in your on hold messaging so that when your potential patients are sitting there waiting in your phone tree, they’re going to say “You know what, it’s probably worth it if all these people said it’s worth it.” That’s just a little piece of information. We’ve used it with a couple of clients and it always really goes over well.
Corey: Yep, we’re the region’s number one ophthalmologist. Don’t just take our word for it. And then you just drop in five of these testimonials.
Jennifer: That’s right, and talking about procedures that maybe your patients didn’t even know you had.
Corey: Mm-hmm (affirmative).
Jennifer: Alright, so what’s the next one, what’s the next one, Corey? I think we’re talking about let’s go into wait time. How do we improve the experience with wait time, because we don’t like to wait.
Corey: Yeah, so obviously sometimes the physicians and the clinic’s just going to run behind. It’s just going to happen. But one of the easiest things to do to improve the patient experience when it comes to wait time is just sort of communicate these clear expectations. And I touched on this a little bit earlier, but when someone comes to check in, if the physician is notorious for running behind, then let them know that when they schedule their appointment and then remind them of that when they come in. And if they’re running really far behind, you may even have to pick up the phone or send a message, if possible, to say “Hey, just so you know, Dr. Smith is an hour and a half behind due to a late surgery.” And try and accommodate folks that way. Because yes, that’s an extra step on your side, but it may mitigate a lot of issues on the flip side when the patient gets there and then they have to sit there for 90 minutes without explanation, especially if they come in, they’re ignored, no one offered them a bottle of water, and then they just sort of sit and stew the entire time.
Jennifer: And you know what happens when you sit and stew, especially if you’re of a certain mindset. What is it? Facebook has more people on Facebook than the population of China. And so when people are sitting, they pull out their phones, their smartphones that they spend an average of 3.3 hours per day on and they’re like “You know, let me pull up my social channel.” And then they’re like “I’m still sitting here.” Then they start communicating about how long they’ve been sitting in your office or take a photo of a piece of trash on the floor, or whatever. And they start communicating with the world via social media and whatever’s happening in your practice has now become something that’s just out there.
Jennifer: So I really think you have to have a plan in place for any kid of long wait times and I think that plan goes back first and foremost to communication, so that you let people know what the expectation is and then kind of a check-in plan if it gets … If a patient is waiting beyond 30 minutes, let’s say that’s your time, then what is your plan B for that patient? At that point do you offer them a bottle of water, or have you gone a step further and this is kind of my next piece here, is do you have a game plan? Why not use something like a restaurant does where you can text them when their appointment is 15 minutes out so they aren’t sitting in the office. But you know for the most part when the doctor’s schedule is opening up or how far behind they are. So why not deploy an electronic device or send them a text message or say “Look, we’re going to keep your appointment, but you’re about an hour behind, so we’re going to let you know when you become about 15 minutes,” so that way they aren’t stuck in your office and they can walk around of something like that. I think that those are things that you could do that are relatively inexpensive that will have a bigger payoff in the end.
Corey: I love that idea of the text message or what have you, like a restaurant, especially as a lot of subspecialties are starting to go into like … You know, like their new offices are going into sort of retail spaces. So we work with an ophthalmologist and they just opened up a brand new office and they’re on the second floor of this mega plaza. So if they’re running behind, then it’s perfectly acceptable for the patients to go downstairs, grab a smoothie, go for a walk, do some light shopping, they get the text that says “Your appointment’s in 20 minutes,” they can start heading back and then go from there. I think that is a fantastic idea.
Jennifer: I totally think so and especially as you see this trend of more folks moving into retail spaces. We have another ortho group that’s in a retail space. I just think it makes sense. And kind of another thing I would do is pay attention to how Uber Health and I think Lyft has a health component, why not consider offering transportation. If an appointment is running really late or maybe a meal voucher if it’s running late over the course of lunch, regardless of monetary recovery, it’s always good to have that plan in place and have a game plan for how are you going to fix it after the fact because yes, everybody’s annoyed that they’re spending too much time in your office, but maybe if somebody spends above 45 minutes waiting for the physician, because you know they’re only going in there for like maybe six minutes with the doctor, maybe, have a plan in place that you’re going to drop a handwritten note in the mail. We’re sorry that you had to wait. Here’s lunch on us. And maybe it’s just a quick gift card to Panera. Because the recovery on that speak volumes, especially if you’re talking about surgical patients or something of that nature.
Corey: Yeah, I mean, if you got a handwritten note from the [inaudible] or the physician, and said that we apologize for any inconvenience and then it came with a $5 Starbucks gift card or something, just think of how many people that patient would say that to because that’s so out of the ordinary.
Jennifer: Well, okay, case in point and then we’ll wrap it up. We were at our company retreat at a big hotel in central Florida this year over on Disney property and the check-in was delayed by about an hour and a half and we had planned the entire retreat around the times working out. And it was a negative experience and we shared it with the staff and they finally got in and I remember we came back from the park and there was a handwritten note apologizing for the inconvenience, as well as a bottle of champagne and some chocolates. And we put that handwritten note on our website, talking about what a way to turn around the experience from our standpoint, and then we’ve told that story over and over again. So handwritten notes are sometimes forgotten about, but they make such a difference and you already know your patients are going to be waiting sometimes. So if they reach a certain threshold, have some handwritten notes ready to go and just pop them in the mail. You actually don’t even need to give something away for free. Just the handwritten note might be enough.
Corey: I agree. Yeah, I think that’s totally … Just the gesture alone. I mean, it was a bonus that we got a box of chocolates when we did that.
Jennifer: Which Danielle ate.
Corey: Yeah. I helped too. But we didn’t need that. If we came back and there was just a note, it would have been like “Oh, that’s really nice,” and that would have been enough of a gesture, I think, to just show that they care and they were paying attention and I believe there’s a photo of that on our Instagram. So at drmarketingtips.com if you guys want to see that.
Jennifer: Awesome. Alright guys, so I think that is plenty of information for today. Everybody’s got to get back to work. So with that, I’m Jennifer.
Corey: I’m still Corey.
Jennifer: And we’ll see you next time on the Dr. Marketing Tips Podcast. Thanks for joining us.
Corey: Thanks, guys.
Speaker 2: Thanks for listening to the drmarketingtips.com Podcast. If there’s anything from today’s show you want to learn more about, check out drmarketingtips.com for our podcast resource center for all the notes, links and goodies we mentioned during the show. If you’re not already a subscriber to our show, please consider pressing the subscribe button on your podcast player so you never miss one of our future episodes. And if you haven’t given us a rating or review yet on iTunes, please find a spare minute and help us reach and educate even more of our medical practice peers. Thanks again for listening, and we’ll catch you next time. Doctor’s orders.
Subscribing and Rating Our Podcast
If you like what you heard, please take a few seconds and subscribe, rate and review our show on iTunes. Here’s how:
Subscribe
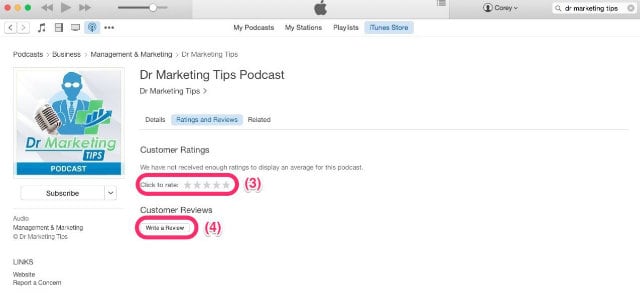
To subscribe, click this link to open iTunes on your computer or press the green “Subscribe” button under the podcast player on this page just above this message. Once you’re in iTunes, you’ll find a “Subscribe” button as denoted by the (1) on the image below. After you’re subscribed, click the “Ratings and Reviews” button (2).
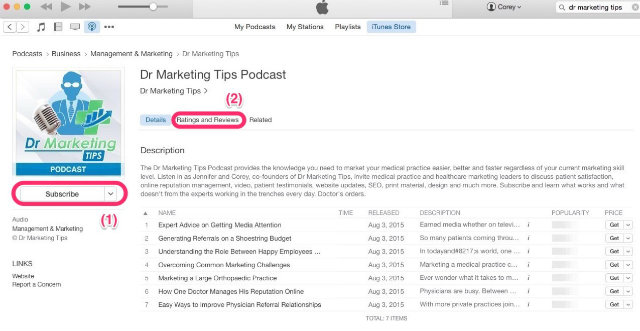
Ratings and Reviews
To leave us a rating and review, select the “Ratings and Reviews” button referenced above (2). Once there, select a star rating for the show (3) and leave your brief review (4).