Engaged patients have better outcomes, lower cost of care, and better overall satisfaction. And a key driver of patient satisfaction is developing a culture beyond clinical care that includes a digital culture of wellness to support practice efficiency, productivity and economic value. It also involves enhancing patient communication, personalization, and engagement.
Engaged patients have better outcomes, lower cost of care, and better overall satisfaction. And a key driver of patient satisfaction is developing a culture beyond clinical care that includes a digital culture of wellness to support practice efficiency, productivity and economic value. It also involves enhancing patient communication, personalization, and engagement.
We recorded this week’s episode live from the 2019 Healthcare Information and Management Systems Society (HIMSS) Global Conference in Orlando where global healthcare thought-leaders gathered to share top-level insights on everything from the patient experience, overall patient engagement, and the influence of AI on the future of healthcare.
Join Jennifer as she shares key takeaways from the conference and breaks down strategies you can use to stay connected to your patients outside traditional clinic walls and between the lines of the care you provide.
Tune in to discover:
- What is the difference between patient experience and patient engagement (or education)
- What your patients actually want
- Where your biggest opportunity to engage patients may lie
- How you can design your processes (care delivery, data flows, etc.) around the patient experience
- How artificial intelligence (AI) is driving the patient experience and the future of healthcare
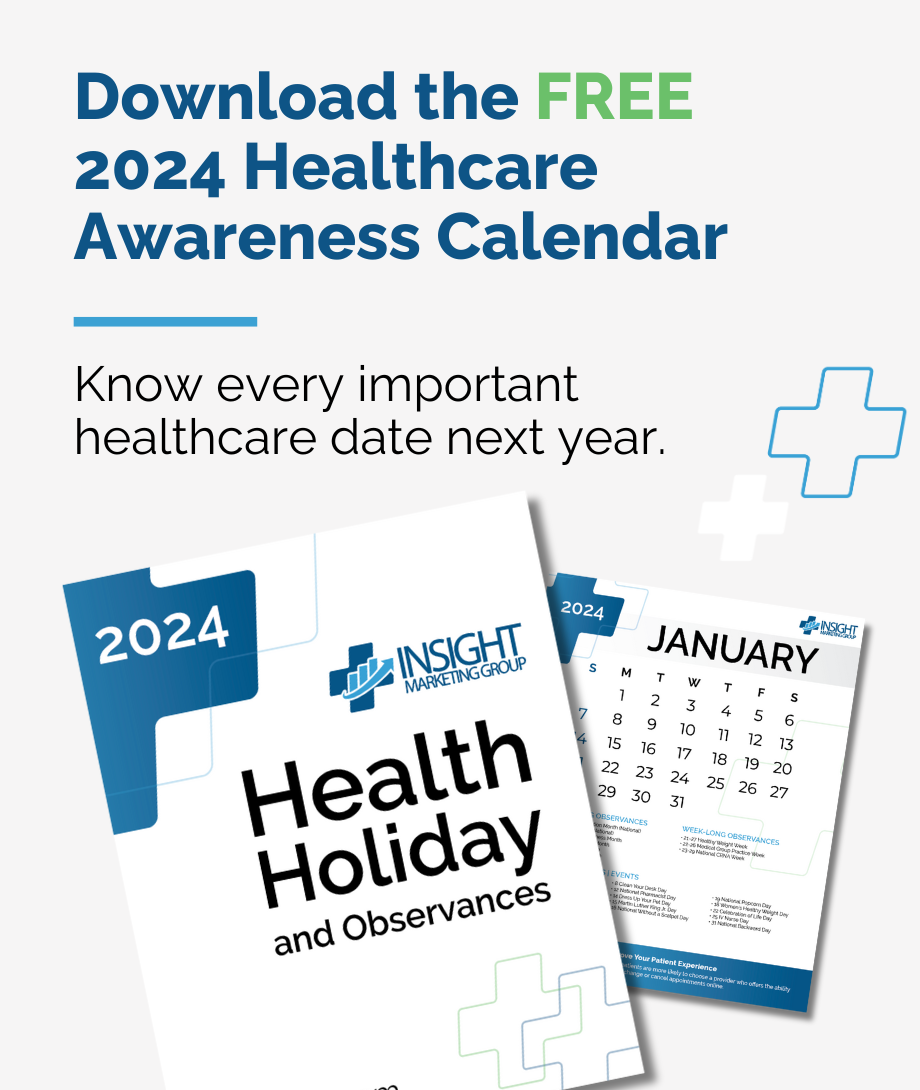
Free Healthcare Awareness 2024 Calendar
Nearly every month of the year has a health holiday or observance, and there are also a number of awareness months that your patients and staff would love to know about. You also don’t want to miss chances to celebrate with your practice’s followers.
Free Healthcare Awareness 2023 Calendar
Nearly every month of the year has a health holiday or observance, and there are also a number of awareness months that your patients and staff would love to know about. You also don’t want to miss chances to celebrate with your practice’s followers.
Transcription
Jennifer: Hey, there. Welcome to the Dr Marketing Tips Podcast. I am Jennifer, and I join you solo this week. In fact, I am recording this episode on the evening of Monday, February 11th after spending a full day today at HIMSS19. The annual HIMSS conference is in my hometown of Orlando, Florida, and since it was so close to home, I thought that I would take the opportunity to go over there and learn as much as possible.
Jennifer: Today, I actually spent an entire day at kind of a preconference summit, leading into the main conference, which is going to last this entire week, and today, I did a deep dive on patient experience and just overall patient engagement. Literally, we started at 8:00 and I walked out the door around 5:15. The folks that were part of the lineup for this day were absolutely amazing, and I’m just going to take a recap of some of the things that I learned, kind of top-level stuff and trying to share it with you, the Dr Marketing Tips audience, but let me just give you kind of an idea of some of the folks that were in the room. We had Jonah Comstock, who is the Editor in Chief of MobiHealthNews. You probably get his emails all the time.
Jennifer: Great publication if you don’t subscribe. We had Adrienne Boissy, the Chief Executive Officer, actually an MD of the Cleveland Clinic, Ms. Karen Murphy, the EVP of Chief Innovation Officer for Geisinger hospitals. We had, you name it, people from Cognizant, the Carilion Clinic. We had President and Chief Executive Officer of Chronic Care Management. We had folks from the co-founder of CipherHealth, Leidos Health, Thomas Jefferson Hospital, Thomas Jefferson University, Jefferson Health, the Behavior Change Design Director from Mad Pow, a rheumatologist from a Wilmington Health, the Chief Experience Officer from Cleveland Clinic, the Chief Medical Officer from Humana.
Jennifer: The head of Uber Health came and spoke to us. The Director of Best Practices from the Cleveland Clinic came. It just went on and on, and what an opportunity to be in that audience and to participate in that dialogue with the rest and just to learn and be able to bring that back to you is such a good experience. Let me just give you kind of my key takeaways from these panels of experts after diving deep in for this last day here. Let’s just get started.
Jennifer: One of the things that kept coming up is, “What is really the difference between patient experience and patient education?” Essentially, experience, patient experience is determined by the patient. It’s their perception of how their experience went with the provider. Engagement on the other hand is what a patient does to actually activate their care, so it’s signing advance directives, filling out paperwork in advance, so we’re very focused from a small or independent practices on improving patient engagement. What really came across as a theme over and over and over is that yes, we’re focused on patient experience, but in order to focus on patient engagement, it’s a two-way, sometimes a three-way street between the clinician, the patient and the practice as a whole.
Jennifer: We have to remember that because a lot of times, what we’re doing from the practice standpoint is we might be putting little things into place to improve patient engagement, which hopefully will improve patient satisfaction scores, but we have to realize that it is a two-way street. Another thing that I heard that I thought was a real interest here is you really shouldn’t need an interpreter to navigate your healthcare, and if you do need an interpreter to navigate your healthcare, a patient advocate, if a patient advocate is necessary, one thing that the one individual kept referencing is that you have to go upstream. Meaning, something might be happening not in your department or with your particular practice, but if it has become so difficult to navigate healthcare, there might be something going on down the road or upstream that you need to go deal with. An example was given of this man and this woman standing on the side of a river, and they kept having to run into the river, grab these people that were drowning, and then pull them over to the shore, and as soon as they would get them to the shore, they would run back into the river and figure it out. Then, by the third try, the guy looks and he can’t find the woman that was helping him anywhere, and here she comes, coming from upstream.
Jennifer: He says, “Where did you go? I needed your help?” She says, “You know what? Finally, it was such a cluster here downstream. I just want to upstream to find out where the problem was”, and I think that really resonates with the practices that we work with on a regular basis. Yeah, we might be dealing with something in the office and it might feel like, especially from patient reviews and whatnot, it might feel like there’s repeated the same kind of problems over and over, and sometimes it’s necessary to take a step back and look upstream and see what you can do.
Jennifer: Another thing that kept coming up in today’s session was, “What is it the patients actually want?” It’s pretty simple. There’s many ways that it was said throughout the day, but essentially, patients want access to your practice, they want ease when it comes to scheduling, and they want simple billing. Essentially, they want to know how much they owe and they want it in big, bold letters. They don’t want to know what the insurance is paying for or what you might end up charging them.
Jennifer: They want to know simple billing, so access, ease of scheduling, and simple billing. Another kind of takeaway from today is that patient engagement. You know what? It’s nothing new. This is old-school stuff. There’s a place for technology and there’s a place for people, and empathy is not a technology tool.
Jennifer: What happens in the white space between the physician visit and the next episode of care, might actually be where we have our biggest opportunity to engage patients, so patient engagement is nothing new and sometimes it’s time to just strip away all the other B.S. that goes along with it and get back to the basics of patient engagement. Another theme that came up was, “When will technology that is expected from consumers within the retail cycle finally make its way over to healthcare?” The good news is, is that consumers, that’s you and I, are finally ready to be engaged via technology, so why not in healthcare? Because technology is ready, and we as consumers, we have been prepared for healthcare to start delivering technology because of these other industries that we interact with on a daily basis. As a provider, what we need to be doing is to design our processes, our care delivery, our data flows, et cetera around the patient experience.
Jennifer: Not try to improve the patient experience around our data flow and our care delivery, it should be the other way around. In fact, it was pointed out that we cannot tell the patient to change what they’re already doing in their everyday life, like what the regular expectations are. The end goal in using technology in the health care cycle is that it should be easy and it should provide seamless healthcare delivery. What they were saying by this is we’re used to getting a reminder on our phone that our packages are being delivered. Why can’t we get the same type of reminder on our phone that we have an appointment coming up next week or that are pills are ready to be picked up, or that we need to go ahead, we’ve been discharged from the hospital and it’s time to make an appointment with your primary care physician.
Jennifer: It’s not seamless in the healthcare cycle like it is on Amazon yet. In fact, we’re working with a very fragmented data within healthcare and big workflow issues. If we want to make a difference in patient experience and overall patient satisfaction and patient engagement, we as practices need to focus on the little changes that can actually make a big difference, so little data, big workflow, but instead, focus on little changes that can make a big difference. One of the really cool things that we talked about today was this delivery, smarter care, an A.I.-driven patient experience. This was a gentleman from, two gentlemen from Jefferson Health that really talked about some of the things that are going on at Jefferson Health, basically, three simple things that we need to do when delivering a better patient experience.
Jennifer: One, we need to focus on access. Meaning that the website needs to be easily accessible, what are we doing with voice automation like Alexa type things, are we easy on mobile, is the follow through easy, things of that nature. Second, we need to focus on experience, take care of not just … Don’t take care of the patient just at the time they’re making that purchase or during the practice, but by surrounding them outside of the practice. It’s like we said before, it’s the stuff between the lines that we have the greatest opportunity.
Jennifer: The gentleman from Jefferson Health was talking about something called, what they would dub as the Angela effect. Basically, you have a nurse in the practice or an MA, and her name’s Angela, and she is this woman that’s been there for years and she remembers your name, she remembers a little bit about your family, she talks to you about how your dog is doing, things of that nature, and they would reference and say, “Well, how do we use AI to go back and create that same Angela effect? Outside of the face-to-face communications, how can we use technology to have that same effect?” Then finally, AI should deliver a convenient experience for the patient. The guys were Jefferson, were talking more and more. I mean super engaging and stuff and they throw out a stat that just blew me away.
Jennifer: By the end of next year, which is Q4, 2020, 75% of aging households will embrace voice assistance. What does that mean? What do patients want? According to the guys from Jefferson, patients want a companion that will walk them through their healthcare journey 24/7. This is how you use AI to provide a simple, comfortable and personable delivery of healthcare.
Jennifer: This is the future of healthcare. What they’re doing over at Jefferson is they have been working to design kind of an Alexa like Bluetooth speaker that goes into every patient room so that when a patient is in there by themselves and they have a question, it’s kind of a closed loop system that’s HIPAA compliant. They can ask their own personal Alexa about maybe the most recent diagnosis they’ve gotten. They want to be able to interact and get a little information. They can do that there.
Jennifer: Maybe the patient isn’t able to change the channel on their television, they can talk to the speaker, the speaker will change the channel. The speaker will dim the lights, the speaker will tell them when the cafeteria opens or closes, when visiting hours are, things of that nature. That’s where AI is going. When it comes to patient engagement, are the patients’ goals aligned with our goals, as in what are we actually trying to get patients to engage in? When we’re talking about patient engagement, we need to be looking at, “Whose goals are we trying to align with? For whose benefit are these goals going to align with, and what are the consequences if our goals don’t align?”
Jennifer: Another part of the challenge when it comes to patient engagement is that we’re using language or terminology that doesn’t necessarily resonate with the patient. We talked about adherence, words like adherence and compliance. An example was given of a clinician seeing this patient and he was diabetic, and his numbers were off, and she said, “Are you taking your pills at noon everyday, Mr Jones?”, and Mr. Jones says, “No, I’m not”, and so she writes that, “Patient refuses to comply with medical recommendation.” It wasn’t that the guy was not complying, granted he wasn’t complying, but what he was doing is they wanted him to take his pills everyday at noon, and that’s when he gets his grandkids from school, and that’s his only hour of the day that he gets to play with his grandkids, so he doesn’t want to fiddle with his medication at noon. Therefore, he might take it at a different time every day, and it affects his outcome.
Jennifer: On the clinician side, we’re using language like adherence and compliance, and not getting down to the nitty-gritty and having these conversations of understanding why somebody may not be adhering or complying to the recommendation that they’re receiving, and so if we want to improve patient engagement and ultimately improve overall patient satisfaction in that experience, even though that experience may be a perceived experience, we have to pay attention to the language and the terminology, and we have to have conversations that lead to those better outcomes. Something that we kept hearing over and over again is that it’s not just about the patient, but it’s also about the clinician, especially as we’re talking about burnout more and more from a physician standpoint. This is kind of a technology conference, so one thing that was said is technology should be able to give clinicians more time to engage with the patient. Technology should not burden our providers. Technology should open up opportunities for our providers to have more time to engage, and clinicians, just like we’re focused on patient engagement, we need to always focus on our provider engagement too because it is a two-way relationships between the patient and the provider.
Jennifer: In fact, data suggest that the moment with the doctor and nurses, that’s the over and over again what drives positive patient experience. Even though our patients only spend about 25% of their visit or less with the actual provider, that 25% can make or break a patient experience and overall satisfaction. That means we need to focus on what provides more time for the clinical staff to spend with the patient. That’s how we improve overall patient experience. The next theme that I was seeing is that data supports that an engaged patient has better outcomes, lower cost of care, and better satisfaction.
Jennifer: In fact, lowest patient engagement, equals the highest financial cost to a provider. We kept hearing like a portal is not engagement, and then something that everyone kept saying over and over as almost as a joke is, “Your patients don’t care about your app. You don’t ask the patients if they download the app and if they actually like it, and logging into a portal is not actually what engagement is most to be. When you’re out there asking patients to engage with you, we oftentimes just assume that all patients want to be engaged in their health, because we’re so focused on engaging. Let’s not assume that people always want to be engaged or that they all want to be engaged in the same way, especially when that engagement is negative.
Jennifer: We need to understand how often the touch points are and what the message is that we’re reinforcing. For example, you have somebody that’s morbidly obese. It’s very difficult to … They know they’re morbidly obese. They know they need to get out there and exercise more. They know they need to take their medication on a regular basis, and we had several examples of providers who would say that they would talk to a patient.
Jennifer: The patient will say, “I didn’t even want to come in here because I get these notifications from you all the time telling me that I need to watch my diet or I need to get out and exercise. I know all these things. I already feel bad enough as it is”, and so it’s important that as a practice, we understand how much people want to be engaged and that we’re engaging on their level at the way that they want to be engaged. Another theme that we talked a lot about was personalization, finding partners within your practice, partners outside your practice that can help you personalize kind of instructions and next steps. One example that was given of, kind of personalization is that a patient using a kiosk to check in and said to somebody it’s very personalized for their experience, and “You should kind of know who this patient is when they come in from one time to the next”, but the patient’s feedback to the provider was, “You care about all this convenience, but the delivery isn’t actually up to par because every time I come in here, I’m filling out the same paperwork on this patient portal. It’s five pages and you’re asking me to fill it out.”
Jennifer: I kind of mentioned it before, but language impacting the patient experience, we use words like problem on the problem sheet versus focusing on solutions, as soon as we tell the patient like, “This is the problem”, versus, “Here’s the possible solution.” Another area where we could focus on patient engagement, one in particular, there’s 44 million adults in the United States that read at an eighth grade level, yet we’re writing most of our healthcare instructions at a sophomore high school level, so a lot of times, people can’t even understand what it is that’s being written, like post-op instructions and things of that nature, and this is the worst in marketing. We do it all the time. We make the font small so that it fits on a single piece of paper, not thinking that we have an aging population base in aging patients and nobody can read those tiny, little fonts, and so if we want to have a more engaged patient that’s active in their healthcare and we want a better patient experience, we’ve got to make it where people can actually read what we’re giving them. Just a couple more here.
Jennifer: The more that we can include the patient in their own care, the higher we can drive patient engagement. Hospitals who have high patient experience, receive higher reimbursements by 50%. What do I mean by including the patient in their own care? At one point, there was a neuroscientist, a neurosurgeon from California, and he was sharing how at his hospital system, he had wanted to bring virtual reality into the system, so those kind of virtual reality goggles that you see people wearing all the time now. He was saying that as a neurosurgeon, typically, the preparation before he has a surgery is that he’ll have a cup of coffee and he’ll look at a chart and he’ll look at some x-rays and look at the CT scans and all of that, and he’ll kind of in his mind plot out his plan of attack to go in there and maybe remove a tumor, but he had this idea that he could adopt virtual reality and create, kind of use virtual reality to see the inside of the patient’s brain, to see the tumors for himself, to physically go in and almost through a simulation, do the procedure several times and figure out what was going to work and what wasn’t going to work.
Jennifer: He had an experience at one point where it was the morning of the surgery, and the patient had signed all the release forms and he went in to do one last trial run through the virtual reality goggles and determined that he wasn’t going to be able to get all the tumor, so he, instead of going through the eyebrow, he went through the side of the skull and was able to get the entire tumor out through the simulation. In order to engage the patient in this effort and to make the patient feel comfortable and the change of care that was being done at the last minute, he put the goggles on the patient and the patient immediately understood because they saw for themselves why something was going to be changed. This neurosurgeon had multiple examples of where he was able to engage the patients in their care using virtual reality, and that increased patient satisfaction scores and reimbursements at his hospital over and over again.
Jennifer: Anytime we can involve the patient in their own care, it’s going to improve patient satisfaction scores. Then, kind of at the end there, the virtual reality talk was one of the best talks of the day and the kind of the emcee of the event got up and said, “What is it that made this audience so hyper-engaged with this particular talk?” The guy was just full of energy. The surgeon was full of energy, and he was very entertaining, he was very data-driven. He used multiple modals of delivery in his talk, so he used video, he used long-form, he used examples, and he told his story.
Jennifer: His narrative was very engaging, and we were engaged because we could see and we could understand his passion in this discussion. Ultimately, that’s what patient engagement was all about, is as providers, we are engaged in the process of making the experiences the best it can be for not just the patients, but for the staff and for the providers themselves, for the clinicians, but we also need the patient to be engaged and we need to provide opportunities for the patient to be engaged in the way that they want to be engaged. When we have engaged patients, ultimately we have higher patient satisfaction. At the end of the day, from a marketing perspective, we’re very focused on patient satisfaction and patient satisfaction scores, and we’re coming full circle again and we’re coming full circle using technology. I mean full circle in that we can have all the technology in the world, but at the end of the day, it’s all about personal connections, feeling like you’re part of something, and being engaged in your overall healthcare means that you’re part of this bigger community for the delivery of overall health and lifestyle changes and things of that nature.
Jennifer: I’m really excited about what the rest of the week is going to hold at HIMSS, and maybe I’ll join you again for another kind of recap of what happens in the sessions. With that, I’m Jennifer, and I really enjoyed. Thank you for coming and visiting me on the Dr Marketing Tips Podcast. Thanks a bunch.
Thanks for listening to the DrMarketingTips.com podcast. If there’s anything from today’s show you want to learn more about, check out DrMarketingTips.com for our podcast resource center with all the notes, links and goodies we mention during the show. If you’re not already a subscriber to our show, please consider pressing the subscribe button on your podcast player so you never miss one of our future episodes. And if you haven’t given us a rating or review yet on iTunes, please find a spare minute and help us reach and educate even more of our medical practice peers. Thanks again for listening and we’ll catch you next time. Doctor’s orders.
Subscribing and Rating Our Podcast
If you like what you heard, please take a few seconds and subscribe, rate and review our show on iTunes. Here’s how:
Subscribe
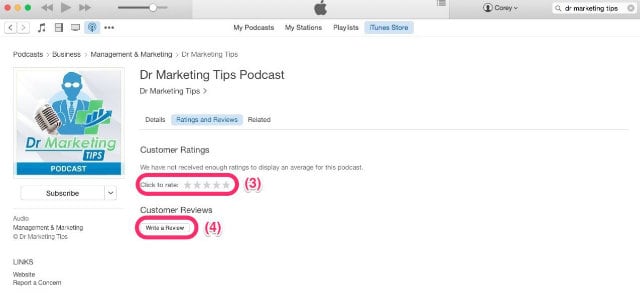
To subscribe, click this link to open iTunes on your computer or press the green “Subscribe” button under the podcast player on this page just above this message. Once you’re in iTunes, you’ll find a “Subscribe” button as denoted by the (1) on the image below. After you’re subscribed, click the “Ratings and Reviews” button (2).
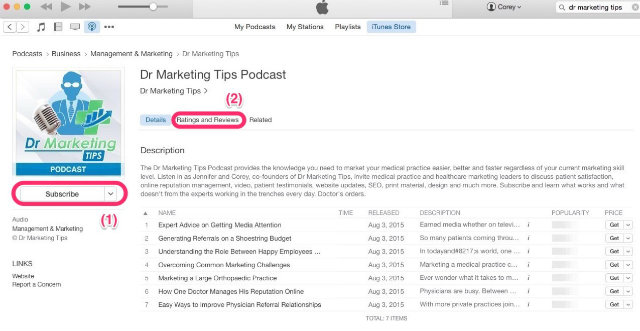
Ratings and Reviews
To leave us a rating and review, select the “Ratings and Reviews” button referenced above (2). Once there, select a star rating for the show (3) and leave your brief review (4).